Little is known about the mechanisms that regulate the growth of the fetus and placenta during protein malnutrition. Eight weeks into your pregnancy or six weeks after conception your babys lower limb buds take on the shape of paddles.
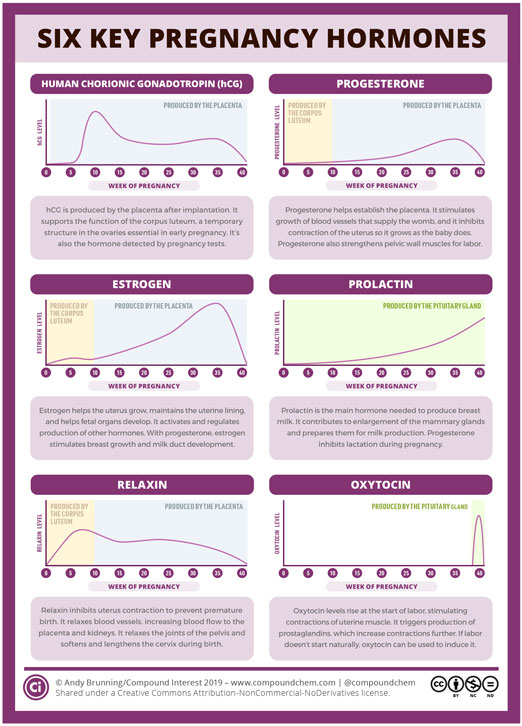 Six Key Pregnancy Hormones American Scientist
Six Key Pregnancy Hormones American Scientist
Glucocorticoids are essential for fetal development Fetus own cortisol and cortisone are the most important hormones regulating fetal tissue maturation.

Fetal development hormones. After ovulation the opened ruptured follicle develops into a structure called the corpus luteum. Fetal development six weeks after conception By the end of the eighth week of pregnancy six weeks after conception your baby might be about 12 inch 11 to 14 millimeters long. These steroids belong to a family of hormones called the glucocorticoids which are known to be associated with the regulation of stress.
Other hormones such as the steroid hormones corticosterone and cortisol are important for fetal development during pregnancy. Hormones play a central role in regulating fetal growth and development. This family of hormones is also known as the steroid hormones or the stress hormones.
The human fetus is dependent upon endocrine development for hormones which support normal development. They act as maturational and nutritional signals in utero and control tissue development and differentiation according to the prevailing environmental conditions in the fetus. Cortisol levels increase continuously during the third trimester and are dramatically elevated in face of anxiety and in chronic stressful conditions.
The other luteinizing hormone LH causes growth and secretion of the testosterone-secreting cells of the male and has an action in controlling the menstrual cycle in the female. Hormone exposure and fetal sex development While your babys chromosomes determine his or her sex medications containing hormones can affect fetal sex development in particular spironolactone a high blood pressure medication that reduces testosterone. This secretes releases the hormones progesterone and estrogen.
Thyroid hormones are intricately involved in the developing fetal brain. The corpus luteum is a temporary structure in the ovaries which produces other key hormones during early pregnancy. One follicle-stimulating hormone FSH causes growth of the main portions of the ovary in the female and the sperm-producing cells in the testis of the male.
Around week 16 GA week 18 the fetal thyroid becomes active enough to support the fetal requirements for neural development. Disruption of the IGF1 IGF2 or IGF1R gene retards fetal growth whereas disruption of IGF2R. Pancreatic Hormones maternal diabetes can affect fetal pancreas development increase in fetal islet beta cells.
The pituitary secretes two other hormones concerned in development. It is known that the placental size and levels of circulating placental hormones such as human chorionic gonadotrophins hCG human placental lactogen hPL and estrogens are affected by the nutritional status of the mother. At 20 weeks the fetus is able to implement feedback mechanisms for the production of thyroid hormones.
The hormonal theory of sexuality holds that just as exposure to certain hormones plays a role in fetal sex differentiation such exposure also influences the sexual orientation that emerges later in the adult. Peripheral endocrine glands thyroid pancreas adrenals gonads form early in the second month from epithelialmesenchye interactions and differentiate into the third month. In the first trimester the developing fetus is initially dependent upon maternal thyroid hormone crossing the placental barrier.
The insulin-like growth factor IGF system and IGF-I and IGF-II in particular plays a critical role in fetal and placental growth throughout gestation. Critical amounts of maternal T3 and T4 must be transported across the placenta to the fetus to ensure the correct development of the brain throughout. Several aspects of placental function are critical for human fetal growth and development including adequate trophoblast invasion an increase in uteroplacental blood flow during gestation transport of nutrients such as glucose and amino acids from mother to fetus and the production and transfer of growth-regulating hormones.
During fetal development T 4 is the major thyroid hormone being produced while triiodothyronine T 3 and its inactive derivative reverse T 3 are not detected until the third trimester. Gonadal Hormones testosterone - required during fetal development for external genital development and internal genital tract in male. The fetal central nervous system is sensitive to the maternal thyroid status.
Estrogens - secreted inactive precursor converted to active form by placenta. Its produced by the placenta after implantation and supports the function of the corpus luteum. The adenohypophysis constitutes 80 of the pituitary gland and houses specialized hormone-producing cells that synthesize and secrete several hormones including but not limited to growth hormone GH thyroid-stimulating hormone TSH follicle-stimulating hormone FSH luteinizing hormone LH prolactin and adrenocorticotropic hormone ACTH.
Human chorionic gonadotropin hCG hCG is an important hormone in early pregnancy. The progesterone helps prepare the endometrium lining of the uterus. Another important family of hormones to the fetuss development are the glucocorticoids like cortisol and corticosterone.
This lining is the place where a fertilized egg settles to develop. Prenatal hormones may be seen as the primary determinant of adult sexual orientation or a co-factor with genes biological factors andor environmental and social conditions.